
Shoulder Pain
Shoulder Joint Complex
The shoulder joint complex includes not only the main shoulder joint (glenohumeral joint) but also the acromioclavicular (AC) joint, which plays an important role in shoulder function and stability. Here’s an overview of both:

Shoulder Joint
The shoulder joint, or glenohumeral joint, is a complex ball-and-socket joint that connects the upper arm bone (humerus) to the shoulder blade (scapula). Here's an overview of its structure and function:
- Bones: The shoulder joint consists of two main bones:
- The humerus: This is the long bone of the upper arm.
- The scapula: Also known as the shoulder blade, it has a shallow socket called the glenoid cavity, which receives the head of the humerus to form the shoulder joint.
- Articular Surfaces: The head of the humerus fits into the shallow glenoid cavity of the scapula, creating the ball-and-socket structure of the shoulder joint.
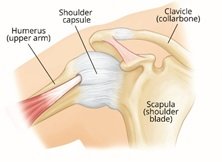
- Joint Capsule: Surrounds the joint and is reinforced by ligaments, providing stability to the shoulder.
- Labrum: A fibrous rim of cartilage around the edge of the glenoid cavity that helps deepen the socket and stabilize the joint.
- Range of Motion: The shoulder joint has the widest range of motion of any joint in the body, allowing movements in multiple planes:
- Flexion: Moving the arm forward and upward.
- Extension: Moving the arm backward.
- Abduction: Moving the arm away from the body to the side.
- Adduction: Moving the arm toward the body from an abducted position.
- Internal Rotation: Rotating the arm inward toward the body.
- External Rotation: Rotating the arm outward away from the body.
- Muscles: Several muscles and tendons surround the shoulder joint and work together to produce movements and stabilize the joint. These include the rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) and larger muscles like the deltoid and pectoralis major.
- Rotator Cuff Tears: Tears in the tendons of the rotator cuff muscles.
- Shoulder Impingement Syndrome: Compression of structures (tendons or bursa) in the shoulder joint.
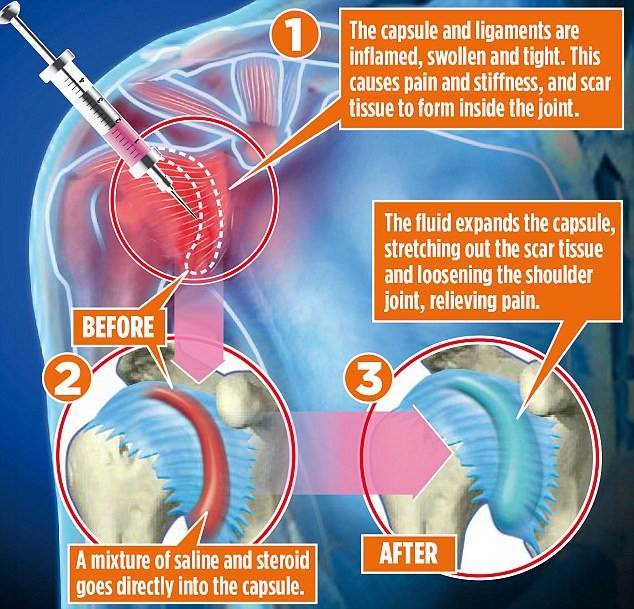
- Frozen Shoulder (Adhesive Capsulitis): Inflammation and tightening of the shoulder capsule.
- Joint inflammation: Inflammation of Shoulder joint/ Acromio-clavicular joint due to local/systemic causes
- Arthritis of Shoulder joint/ AC joint: Degenerative changes in the joint, such as osteoarthritis or rheumatoid arthritis.
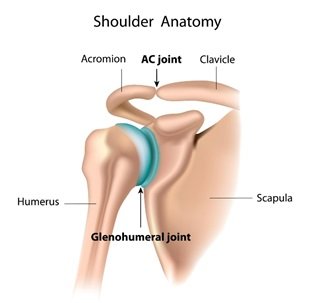
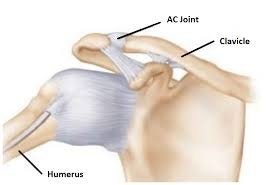
Acromioclavicular (AC) Joint:
- Articular Surfaces: The AC joint is formed by the acromion (a projection of the scapula) and the clavicle (collarbone), which articulate with each other.
- Ligaments: Several ligaments, including the acromioclavicular ligament and coracoclavicular ligaments (trapezoid and conoid ligaments), provide stability to the AC joint.
- Stability: The AC joint helps to transmit forces from the arm to the rest of the body and supports movements of the shoulder complex.
- Shock Absorption: It absorbs shock and distributes forces during activities like lifting and carrying.
- AC Joint Separation: Injury to the ligaments that stabilize the joint, often due to trauma or overuse.
- Arthritis: Degenerative changes within the AC joint, leading to pain and stiffness. Common in weight lifters
- Impingement: Compression of tissues around the AC joint, causing pain and restricted movement.
Frozen Shoulder
Adhesive capsulitis, also known as frozen shoulder, is an inflammatory condition characterized by shoulder stiffness, pain, and significant loss of passive range of motion.
Primary adhesive capsulitis is typically idiopathic and has a gradual onset. It is often associated with underlying conditions such as diabetes mellitus, thyroid disease, drugs, hypertriglyceridemia, or cervical spondylosis.
Adhesive capsulitis has a prevalence of approximately 2% to 5% in the general population, with a mean onset of age of 55. There is a slightly more significant predominance in females, and the non-dominant hand is often affected. Patients with autoimmune comorbidities, such as thyroid disorders and diabetes mellitus, are more prone to developing adhesive capsulitis
Diagnosis
During a physical exam, patients with adhesive capsulitis may exhibit a decreased glenohumeral Range of Movements(ROM) and experience pain during testing. Pain will often limit a complete and thorough physical exam. Typically, there is a significant reduction in the active and passive ROM in 2 or more planes of motion compared to the unaffected side. The loss of ROM usually follows a specific pattern starting with external rotation, followed by abduction, internal rotation, and forward flexion.
Magnetic resonance imaging may show rotator interval synovitis, hypertrophy of the coracohumeral ligament, loss of the subcoracoid fat triangle, and thickness of the glenohumeral joint capsule. Ultrasound of Shoulder joint is very promising and eliminating the need for MRI.
Treatment:
1. NSAIDS/Physical Therapy
2. Hydrodilatation: With this treatment modality, the glenohumeral capsule is injected with saline to promote capsule dilation. This treatment approach benefits in reducing pain and improving ROM and function, helps in faster recovery.
Rotator Cuff Tears
The most common tendon involved in tears is the supraspinatus tendon, but tears can also affect other parts of the rotator cuff.
- Fraying: Many tears start as small frays or partial tears due to wear and tear over time. This can be caused by repetitive overhead motions or aging-related degeneration of the tendon tissue. This can be treated with Regenerative therapy (Platelet Rich Plasma), supports healing of the tear.
- Progression: As the damage worsens, If untreated or under continued stress, such as lifting heavy objects, a partial tear can progress to a complete tear.
- Pain: Persistent pain in the shoulder, especially with overhead movements or lifting.
- Weakness: Difficulty or weakness when lifting or rotating the arm.
- Limited Range of Motion: Difficulty reaching overhead or behind the back.
- Diagnosis: Diagnosis is typically made through physical examination, imaging tests (like MRI), and sometimes diagnostic injections to confirm the tear.
- Treatment Options: Treatment depends on the severity of the tear:

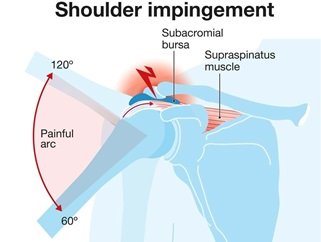
Shoulder Impingement Syndrome
Shoulder impingement syndrome occurs when the tendons of the rotator cuff muscles or the bursa become compressed or irritated as they pass through the narrow space between the bones in the shoulder.
- Anatomy: The space between the top of the upper arm bone (humerus) and the acromion (part of the shoulder blade) can narrow due to bone spurs, inflammation, or thickening of the tendons or bursa.
- Repetitive Movements: Activities that involve repetitive overhead movements (such as painting, swimming, or throwing) can lead to wear and tear on the tendons and bursa.
- Shoulder Instability: Weakness or imbalance in the muscles of the shoulder can lead to abnormal movement and increase the risk of impingement.
- Pain: Pain is typically felt on the outer aspect of the shoulder, especially when lifting the arm overhead or reaching behind the back.
- Weakness: Weakness or loss of strength in the shoulder muscles, particularly when lifting objects or performing overhead activities.
- Stiffness: Stiffness and limited range of motion, especially in activities that require reaching or lifting.
- Physical Examination: Your doctor will perform a physical exam to assess shoulder range of motion, strength, and tenderness.
- Imaging Tests: X-rays can show bone spurs or changes in the structure of the shoulder joint. MRI or ultrasound may be used to visualize soft tissues like tendons and bursa.
Treatment:
PROLOTHERAPY is found to be effective to relieve impingement symptoms and healing.
 +91 8248827895 |
+91 8248827895 |  absolutevitalhealth@gmail.com
absolutevitalhealth@gmail.com
 Joint Pain
Joint Pain