Nerve Pain
Most common causes:
Postherpetic neuralgia (PHN) is nerve pain that develops after a shingles (herpes zoster) infection, following the pattern of a specific skin area (dermatome). This type of pain can be severe and greatly affects a person’s quality of life and ability to function at home and in society.
Varicella is a viral infection that may lead to varicella zoster (chicken pox) on first exposure and subsequently remains in a latent phase for the majority of lifetimes. HZ develops secondary to reactivation of varicella virus from its latent state. Varicella virus is kept in a latent state by the body’s cell-mediated immunity. When there is a decrease in cell-mediated immunity, the risk for reactivation and subsequent HZ increases

Acute Herpes Zoster And Post Herpetic Neuralgia
Around 10% to 20% of people who have had shingles (herpes zoster) experience ongoing pain, known as postherpetic neuralgia (PHN), even after the initial infection has resolved.
The incidence of PHN developing from HZ also increases with age. Patients older than 70 years with HZ have a 50% risk for the development of PHN, whereas it rarely develops in patients younger than 40 years. Several factors increase the risk of developing postherpetic neuralgia (PHN), including older age, more severe rash during the initial infection, being female, and experiencing more intense pain during the acute phase of shingles.
Post-herpetic neuralgia is mostly diagnosed based on clinical signs. Typically, a patient will report ongoing pain in a specific area of their skin, aligned with a dermatome, which is the region of skin supplied by a single nerve root. Initially, herpes zoster (shingles) presents with a rash that forms blisters, crusts over in 1 to 2 weeks, and causes burning, increased sensitivity, itching, and intense pain. Before the rash appears, patients may experience symptoms like headache, fever, tiredness, unusual skin sensations, and sensitivity to light (photophobia).
Postherpetic neuralgia (PHN) can develop about 2 weeks after the onset of herpes zoster (shingles) and represents the chronic phase of the disease. It's characterized by severe pain that includes burning sensations, abnormal sensations (dysesthesia), itching (pruritus), and heightened sensitivity to touch (allodynia) or tingling sensations (paresthesia) in the affected dermatome. Typically, the pain improves or goes away within 6 months, but in some cases, it can persist for years, causing significant disability and discomfort.
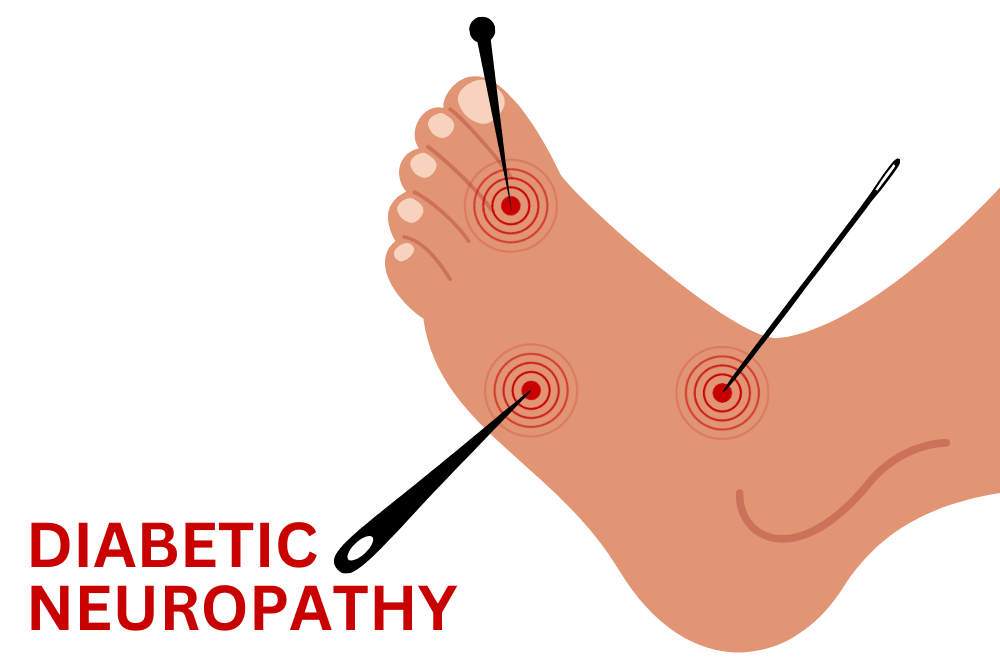
Diabetic Neuropathy
In developed countries, diabetic neuropathy induced by diabetes mellitus (DM) is one of the most common types of nerve damage. It can occur due to the toxic effects of high blood sugar directly affecting nerve cells. Additionally, both central and peripheral nerve structures can be damaged, often accompanied by dysfunction in the small blood vessels that supply the nerves (vasa nervorum).
More than 80% of patients with diabetic neuropathy experience symptoms that are distal (starting in the feet or hands) and symmetric (affecting both sides similarly). Initial symptoms typically include reduced sensation, a burning sensation in the feet (especially at night and aggravated by touch), tingling in the feet, and occasional shooting pain.
Treatment includes Pharmacological treatment ( Medications such as Neuropathic Pain Medications, Opioids) and Interventional management (Spinal Cord Stimulator)
 +91 8248827895 |
+91 8248827895 |  absolutevitalhealth@gmail.com
absolutevitalhealth@gmail.com
 Joint Pain
Joint Pain